If you’ve considered getting your practice recognized as a
Patient-Centered Medical Home, you’ve no doubt taken a look at the standards.
There are several programs you could consider to get your practice PCMH "certified," and they all have some benefits, but for today, let’s talk about the National Committee on Quality Assurance’s
(NCQA) PCMH program.
Of course, maybe we steer the conversation in that direction
because that’s the one we happen to have built a tool around. (That always
helps.) But we are fairly unbiased when it comes to how your practice chooses to
get recognized. In fact, we are building PCMH tools that will
work with whatever program you’re using for certification.
PCMH Recognition
Back to NCQA, if you’ve taken some time to look over this
program, you’ll see there are 6 Standards, with 28 Elements (6 of which are
must-pass), with nearly 150 sub-factors, some of which are considered critical
factors. And NCQA is a documentation-based system. That means each of
these subfactors require documentation to prove that
you’re actually doing them. In fact, some factors will require more than one document! You can do the math and determine that's a lot of documentation. It's enough to make
a busy practice manager head for the hills.
Although there can be a lot of work involved in getting
recognized as a PCMH, it is do-able. And it doesn’t mean shutting down your
practice to get it done.
In fact, it’s just the opposite.
PCMH is about building relationship with patients, not
wasting time you don’t have on one more administrative burden.
That’s why we built the BizMed Online PCMH Tool. It’s sort
of like a PCMH Project Manager, Documentation Development Tool, Documentation
Storage Unit, and PCMH Score Tracker all in one!
The best news of all? It’s absolutely free.
Getting Started
The first step is to follow our easy step-by-step instructions on registering for the BizMed’s Toolbox.
After you’re done with that, it’s a good idea to take the
PCMH Express Assessment.
Then you’re ready to get started.
PCMH Score Tracking
When you go through the tool you’ll notice that the Toolbox
will display your practice name. Underneath your practice names you can see the
tools available to you by clicking on the triangle. There you will see we’ve
included NCQA Requirements you can review as you go through the process. There
are also free examples of documentation you can use for your practice as well.
Do you see how the Summary Status Report provides the
practice with a score and includes a status bar at the top of the screen?
That’s because this practice has gone through each element and indicated which
documents it would be providing. The system then tracks what documents have
been uploaded and keeps the practices updated on its’ progress.
This is a handy report you can use if you need to update
external entities about your progress. Simply click on “Print Summary” to have
a copy ready to share with others or to create a PDF version of the report to
keep in your files (A copy will be automatically saved to your PCMH documents toolbox).
Click on each tab, beginning with PCMH1 and expand each
element to review the sub-factors and odd documentation.
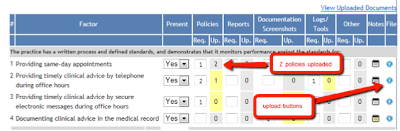
In the “present” column, you can select Yes/No/NA for each
factor your practice is choosing to address. Remember, you don’t have to do
each of these factors to receive NCQA recognition.
You need all 6 Must Pass Factors (1A, 2D, 3C, 4A, 5B, and
6C), and then you need the following points to receive Level 1, Level 2, or the
highest Level 3 recognition:
- Level 1 recognition: 35 – 59 points (plus all 6 must-pass elements)
- Level 2 recognition: 60 – 84 points (plus all 6 must-pass elements)
- Level 3 recognition: 85 – 100 points (plus all 6 must-pass elements)
We encourage you to go through the tool, element by element,
to consider which items you’re doing already, and then go back to the Summary
screen to see where you’re at on the Must Pass elements and the overall score.
If you like what you see, then you can begin on preparing documentation. If
you’d like to achieve a higher score, then consider what areas you’d like to
focus on.
Any time you’re going through the BizMed PCMH Application
Tool and you’ve forgotten the NCQA requirements, simply click on the “info”
icon to the left of the element name and the document will open in a new
browser tab.
You can also add Evaluation Notes for NCQA for each Element
by clicking on the comment “Note” icon next to the Element Title. When content
is added to an evaluation note, the icon changes color from gray to blue.
The application will automatically calculate your score for
the Element based on the NCQA rules and weights. Please note that most often
Factors are weighted differently. Refer to the NCQA documentation for
explanatiosn of the calucation algorithms.
In the adjacent 5 columns you can estimate the number of
individual documents required to substantiate the Factor is present. There are
5 document types available: Policies, Reports, Screenshots, Logs/Tools, and
Other. Your estimate is entered in the “Req.” (required) column for each.
Creating a PCMH Baseline Assessment
Once you’ve done this for each of the elements, we encourage
you to click on "Print Summary" or "Print with Details" which will save a copy of your Summary Status Report as a Baseline Assessment in your documents folder. Why?
Having a baseline can be critical for showing progress made in the practice.
Throughout the project you may add additional PCMH features to your practice.
Having something to go back to to demonstrate progress can be very helpful!
PCMH Documentation – Getting it Done!
You can now begin to upload the required cocuemntation by
clicking on the blue round icon on the right of each row. A popup will display
allowing you to select a document to upload. Make sure you select the correct
document type from the drop-down menu!
You may also designate if the document you are uploading is Primary, Secondary, or just Supporting. You may select certain pages and rename the document if needed. Close the Upload screen when you’re finished.
You may also designate if the document you are uploading is Primary, Secondary, or just Supporting. You may select certain pages and rename the document if needed. Close the Upload screen when you’re finished.
If you have one document that works for several factors, you
only have to upload it once! You can choose to link an already uploaded
document to other factors.
The screen will update to reflect the number of documents
uploaded. Please note that if the number of documents uploaded (or linked) is
not sufficint to satisfy the requirements, the cell will light up in yellow.
To view uploaded documents for your elements, click on the
“Vew Uploaded Documents” link.
A popup screen will display listing all documents linked to
this element.
You can also add private Notes to each factor to share with
others or for your own use. Simply click on the notepad icon.
If you’re working with a consultant or facilitator, you can
allow them access to review your completed application. A section for reviewer
notes have been included along with a checkbox for them to mark when the
element is complete.
Sometimes you’ll notice a “Note” icon appear next to a
Factor. This means that NCQA has REQUIRED additional information. Click on the
note to add the necessary information. The icon will change color to indicate
that content has been added.
While the Summary tab provides you with an overall view of
practice progress, the “NCA Submission” folder on the left displays all the
documentation accumulated so far, including all Notes. This is where you can
delete uploaded documents by clicking the red “X” next to the document name.
Please note, this action cannot be undone.
You can print summary and detail status reports from the Summary
page at any time. A copy will always be saved to your PCMH Documents folder for
your records.